Clinical Education
Our curriculum provides a broad clinical fund of knowledge and unique educational experiences, based upon a resident's individual interests.Our residents develop their clinical expertise through a combination of conferences and rotations. There are two dedicated resident conferences per day, covering all subspecialties of neurology. These sessions are teleconferenced to all teaching hospitals and recorded for later review by residents on nightfloat rotations, vacation, or in self-guided study. Clinical teaching is provided on the required inpatient rotations in neurovascular, neurocritical care, epilepsy, general neurology, consultation, and pediatric neurology, as well as during required outpatient rotations in general and subspecialty neurology clinics and pediatric neurology.
Residents have abundant opportunity to explore their specific interests with more than 42 weeks of elective time for each resident. Clinical electives are available in cognitive neurology, movement disorders, neurodegenerative disorders, neuromuscular disorders, epilepsy, EMG, EEG, intra-operative monitoring, sleep, multiple sclerosis, neuro-oncology, neuroradiology, interventional neuroradiology, neuropathology, neurocritical care, neurovascular neurology, headache disorders, and general neurology.
Weekly Lecture Schedule
As a tertiary referral center for more than four states, our Neurology residents at the Hospital of the University of Pennsylvania care for patients with common and rare neurologic diseases. Our residents learn to diagnose and manage these patients under the supervision of an outstanding faculty, recognized as national experts in their field. In addition to clinical exposure, resident education is augmented by conferences from the same faculty discussing the most recent advances in neurology. The first 3 months of lectures are focused on neurological emergencies, outpatient neurology, neurodiagnostic studies, and pediatric neurology. During the remainder of the academic year the sub-specialty neurology curriculum is designed to enhance to enhance fund of knowledge and clinical reasoning.Weekly Clinical Schedule
Typical PGY-2 Schedule On The Ward Service* PGY-2 residents on the Ward Service are OFF every other weekend and one weekday every other week
M
|
T
|
W
|
Th
|
F
|
Sa
|
Su
|
|
|---|---|---|---|---|---|---|---|
7:00
|
Signout & Preround
|
Signout & Preround
|
Signout & Preround
|
Signout & Preround
|
Signout & Preround
|
* Off
|
* Off
|
8:00
|
Career Curriculum |
Morning Conference
|
Professor's Rounds | Morning Conference | Morning Conference | ||
9:30
|
Teaching Rounds
|
Teaching Rounds
|
Teaching Rounds
|
Teaching Rounds
|
Teaching Rounds
|
||
12:00
|
Admin Meeting
|
Noon Conference
|
Noon Conference
|
Noon Conference
|
Noon Conference
|
||
1:00
|
Patient Care | Patient Care | Patient Care |
Patient Care
|
Patient Care | ||
5:00
|
Signout
|
Signout
|
Signout
|
Signout
|
Signout
|
Typical PGY-4 Schedule On The Ward Service
Preliminary interns at Pennsylvania Hospital (ERAS ACGME ID: 1404111376) receive a more focused experience in general medicine. Training takes place entirely at Pennsylvania Hospital, with the exception of the inpatient and outpatient neurology experiences. There are daily internal medicine conferences. Rotations are divided between inpatient medicine (7 blocks), ICU (2 blocks), and electives (3 blocks).
| M | T | W | Th | F | Sa | Su | |
|---|---|---|---|---|---|---|---|
| 7:00 | Signout & Discharge Planning | Signout & Discharge Planning | Signout & Discharge Planning | Signout & Discharge Planning | Signout & Discharge Planning | OFF | OFF |
| 8:00 | Career Curriculum | Morning Conference | Professor's Rounds | Morning Conference | Morning Conference | ||
| 9:30 | Teaching Rounds | Teaching Rounds | Teaching Rounds | Teaching Rounds | Teaching Rounds | ||
| 12:00 | Admin Meeting | Noon Conference | Grand Rounds | Noon Conference | Noon Conference | ||
| 1:00 | Patient Care | Patient Care | Patient Care | Patient Care | Patient Care | ||
| 5:00 | Overnight Home Call | Signout | Overnight Home Call | Signout | Signout |
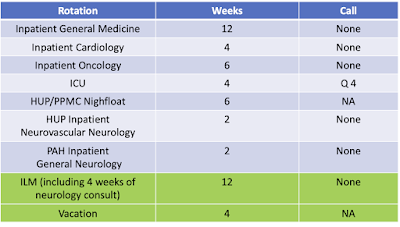
Yearly Clinical Schedules
PGY-1
We are committed to optimizing your neurology experience and career development starting from the moment you match into the University of Pennsylvania Neurology Residency program. At the beginning of your preliminary internship, regardless of where that is completed, we assign you a neurology faculty mentor with shared career interests. We have further integrated neurology training into the PGY-1 year for those trainees who pursue their preliminary medicine internship at one our Penn-affiliated sites:
- The Hospital of the University of Pennsylvania (ERAS ACGME ID: 1804121102)
- Pennsylvania Hospital (ERAS ACGME ID: 1404111376)]
Interns receive early exposure to neurology in addition to outstanding training in internal medicine. During the prelim year, residents are exposed to inpatient and outpatient neurology through the following experiences:
- 2-weeks of Neurology at Pennsylvania Hospital on a small inpatient service, call free, weekend free
- 4-weeks of Neurology at The Hospital of the University of Pennsylvania performing consults, call free, weekend free
- 2-weeks on The Hospital of the University of Pennsylvania Neurovascular service, call free
- PGY-1 residents see outpatients in the Neurology resident clinic on average once per month, where they work with an assigned PGY-4 neurology resident mentor, whose clinic they ultimately inherit.
- Trainees receive lumbar puncture instruction in the outpatient clinic under faculty supervision, on average once per month
- During elective blocks, there are opportunities to pursue inpatient and outpatient clinical neurology electives or laboratory work for research-focused trainees.
Preliminary interns at The Hospital of the University of Pennsylvania internal medicine program (ERAS ACGME ID 1804121102) will have in-depth experiences in both general medicine and subspecialty medicine. Trainees spend the majority of their inpatient medicine time at The Hospital of the University of Pennsylvania with the remaining 2 months at the Penn Presbyterian Medical Center or The Corporal Michael J. Crescenz Philadelphia Veterans Affairs Medical Center. In addition to patient care provided by trainees, there are non-housestaff services at all three hospital sites. There are daily internal medicine conferences in addition to dedicated daily teaching sessions prior to morning rounds. The program is on a 6+2 block scheduling system. Trainees spend up to 6 weeks in a row on inpatient services, followed by 2 weeks in the ambulatory or elective setting called Individual Learning Modules (ILM).
PGY-2
The PGY-2 residents provide most of the direct inpatient care and in-house night-time coverage of the Hospital of the University of Pennsylvania, Pennsylvania Hospital, and Presbyterian Medical Center. The services at the Hospital of the University of Pennsylvania are covered with a mixture of overnight call and nightfloat systems while the services at Pennsylvania Hospital and Presbyterian Medical Center are primarily covered with a nightfloat system. Overnight, the PGY-2 residents discuss all cases with a PGY-3 or PGY-4 supervising resident. Multiple subspecialty attending neurologists—including critical care, neurovascular, and epilepsy—are on-call each night to discuss complicated cases. This system maximizes resident autonomy while balancing patient care, resident education, and resident lifestyle. All PGY-2 residents have at least 10 weeks of elective time that is customized to the interests of the trainee, as well as 4 weeks of subspecialty outpatient experiences so that our residents have the early exposure to all areas of neurology necessary to make well-informed Fellowship decisions. Our PGY-2 resident schedule is on a 6+2 block scheduling system. Trainees spend up to 6 weeks in a row on inpatient services, followed by 2 weeks in the ambulatory or elective setting, or on vacation.PGY-3 and PGY-4
During the PGY-3 and PGY-4 years, residents divide their time evenly between inpatient and outpatient/elective opportunities. Their role on the inpatient adult neurology services is to oversee patient care provided by the PGY-2 residents and teach neurology to the PGY-2 residents and the University of Pennsylvania Perelman School of Medicine neurology clerkship students. In addition to daytime supervision, our PGY-3 and PGY-4 residents provide both overnight in-person or home-call supervision of our PGY-2 residents. This system prepares PGY-3 and PGY-4 residents for the home-call responsibilities they will have as an attending neurologist. In addition to outstanding adult neurology training, our PGY-3 and PGY-4 residents have the incredible opportunity to learn inpatient and outpatient pediatric neurology at one of the nation’s preeminent children’s hospital in the United States, the Childrens Hospital of Philadelphia (CHOP).
PGY-3 and PGY-4 residents have complete autonomy to pursue elective opportunities in any subspecialty of neurology, choosing to provide neurologic care in Tanzania under the supervision of our faculty, perform research, or serve as a teaching assistant in the preclinical neurology course at the University of Pennsylvania Perelman School of Medicine.